In a recent article published in The Lancet Microbe, researchers discussed the World Health Organization (WHO) ‘s fungal priority pathogens list (FPPL). They shed light on the disparities between the list’s ranking and the actual fungal disease burden and proposed a revised prioritization list addressing regional disparities.
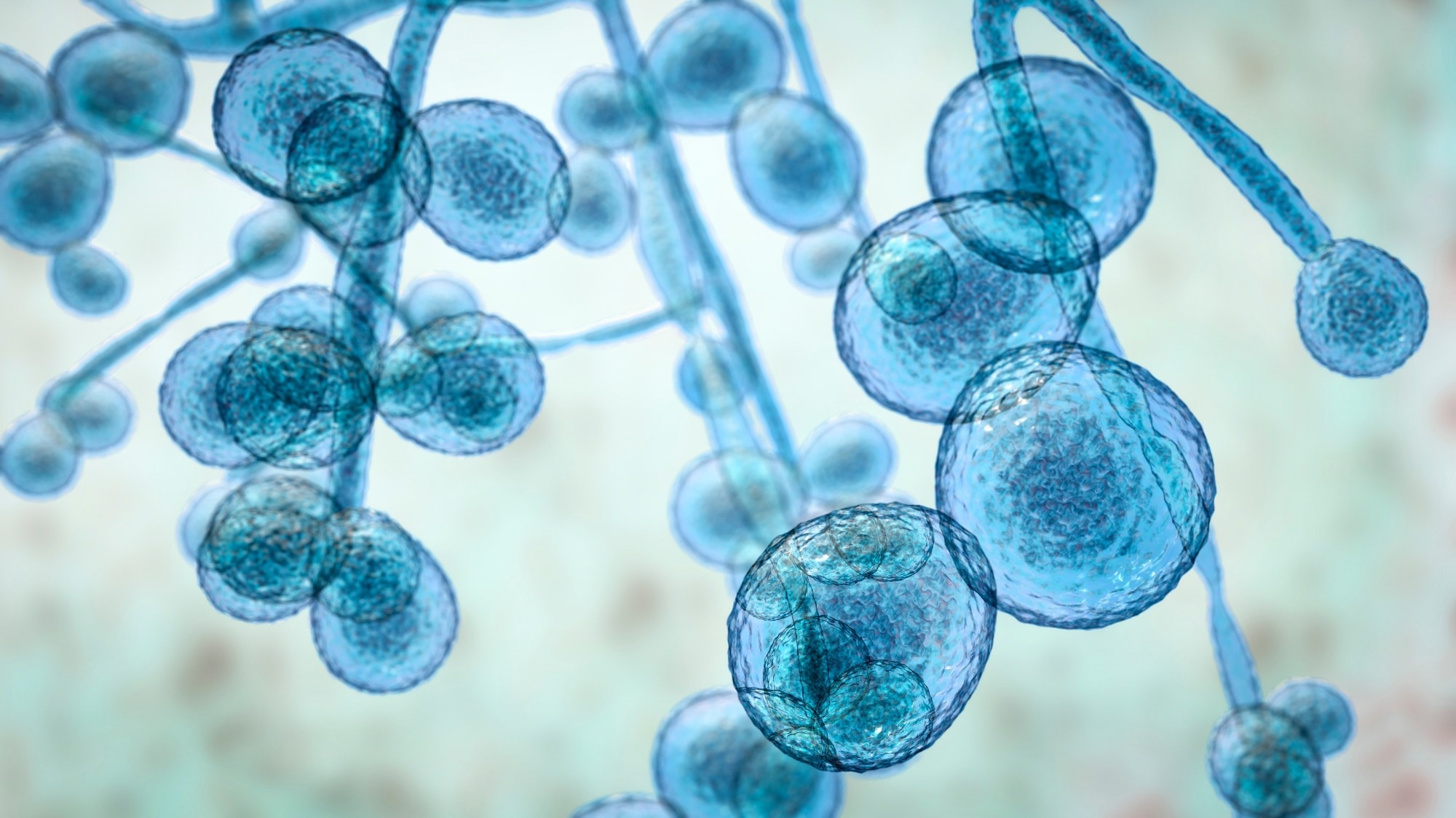 The WHO fungal priority pathogens list: a crucial reappraisal to review the prioritisation. Image Credit: Kateryna Kon / Shutterstock
The WHO fungal priority pathogens list: a crucial reappraisal to review the prioritisation. Image Credit: Kateryna Kon / Shutterstock
Background
WHO published the first fungal priority pathogen list in October 2022 to address the challenges in fungal disease diagnosis, treatment, and research. The prioritization process involved systematic reviews, expert opinions, and consideration of specific criteria, leading to the establishment of intensity levels for each pathogen. The final ranking was determined through surveys and scaling methods, highlighting the urgency of addressing fungal infections alongside bacterial resistance.
While recognizing the importance of the WHO FPPL, researchers in the present study suggest that it may inadequately represent the burden of certain fungal pathogens and propose revised prioritization.
Mucorales
Though classified as a high-priority group by WHO, Mucorales may pose a greater threat than currently acknowledged. The incidence of mucormycosis surged during the coronavirus disease 2019 (COVID-19) pandemic, particularly in India, with estimates far surpassing those of high-income countries. Diabetes emerges as the primary risk factor. The rising diabetes burden in India and Southeast Asia suggests a potential surge in mucormycosis cases in the region. Diagnostic challenges and treatment uncertainties further compound the threat, necessitating robust research and public awareness efforts.
Candida spp.
Candida spp. infections affect over 600,000 annually, with a mortality rate of 30–40%, but their prioritization in the FPPL may not fully reflect their clinical significance. Candida glabrata and Candida parapsilosis, associated with lower priority levels, are gaining recognition due to emerging antifungal resistance and biofilm-production capabilities, respectively. Concerns about fluconazole-resistant strains of C. parapsilosis leading to hospital outbreaks with high mortality rates highlight the need for infection control efforts.
Histoplasma spp.
Histoplasmosis, caused by Histoplasma capsulatum, exhibits a broader global distribution than previously recognized, with new disease foci observed in North America, Africa, and Europe. A study reported a high incidence of histoplasmosis across the United States, suggesting widespread endemicity. However, inadequate diagnostic capacity and low clinical suspicion contribute to underdiagnosis and underreporting, particularly in Africa and Southeast Asia. Improved access to diagnostic tools and antifungal therapies is crucial to address histoplasmosis.
Fusarium spp. and eumycetoma causative agents
Fusarium spp. infections are rare and affect highly immunocompromised individuals, with incidence rates not exceeding 6%. Despite uncertainties in optimal treatment strategies and the potential future increase in susceptible populations, Fusarium infections pose a lower global threat compared to mucormycosis or candidemia. Similarly, eumycetoma, though lacking precise global incidence data, is a significant concern in low- and middle-income countries due to high morbidity rates, limited treatment guidelines, and frequent relapses.
Coccidioides and Paracoccidioides spp.
Coccidioidomycosis is expanding its endemic areas due to climate change, with significant underreporting due to a lack of notifiable status in many regions. Paracoccidioidomycosis, prevalent in South and Central America, faces diagnostic challenges due to taxonomic revisions and limited surveillance. Lomentospora prolificans and Scedosporium spp., though rare, present nosocomial risks, yet their prioritization over coccidioidomycosis and paracoccidioidomycosis seems disproportionate, considering their lower incidence and public health impact. Talaromyces marneffei, endemic in Southeast Asia, poses a serious threat to immunocompromised individuals, highlighting the urgency for improved diagnostic tools and research attention.
Cryptococcus spp.
Cryptococcus neoformans, a common cause of cryptococcal disease in immunocompromised individuals, particularly those with advanced human immunodeficiency virus (HIV) infection, results in significant morbidity and mortality worldwide. Conversely, Cryptococcus gattii, once considered endemic to specific regions, has shown global spread and presents unique clinical challenges, warranting a higher priority status. Pneumocystis jirovecii is responsible for pneumonia primarily in immunocompromised populations.
Proposal for the improvement of WHO FPPL
The uniform approach of the FPPL does not consider the varied nature and distribution of fungal infections. To address this, the researchers propose region-specific customization of priorities using WHO regions as a proxy. They suggest four major pathogens for crucial prioritization globally: Cryptococcus, Aspergillus spp., Candida spp., and Pneumocystis jirovecii. Additionally, they advocate for adjustments in prioritization based on regional considerations. For example, Coccidioides and Paracoccidioides spp. should be considered high-priority pathogens in the Americas, while Mucorales may warrant critical prioritization in Southeast Asia and the Eastern Mediterranean. Histoplasma spp. should also be prioritized higher in the Americas and Africa. Furthermore, Talaromyces marneffei should receive higher prioritization in Southeast Asia and the Western Pacific regions. Pathogens with lower disease burdens may be placed in the medium-priority group.
Conclusion
The FPPL is a commendable global initiative but lacks customization based on geographical regions, potentially overlooking the true threat posed by certain fungal pathogens in specific areas. Efforts to address these challenges are crucial to enhance global awareness, research, and, ultimately, control of fungal infections.